
“What Could Have Made Your Job Easier Today?” — Front-Line Staff vs. Barcode Scanners
Barcode scanners in the hospital are used daily for most patients. Nurses scan every medication, infusion, lab, fluid, and blood given to a patient. Many patients have multiple medications at a time, some of which are administered multiple times a day. Factoring for our volume of patients, the number of times barcode scanners are used climbs into the thousands on any given week.
These scanners are critical in the delivery of efficient, quality care. They have to work every day, in every instance. Their failure to function means a delay in delivering care, frustrates staff, and costs the institution time that could be better spent. Simply put: It’s wasteful.
When we talk about waste, we’re talking about “muda” — a Japanese term used in lean process thinking. Waste is more than the physical, though. Written on a giant dry-erase board in the Nerancy Neuroscience Intensive Care Unit (NNICU): “Waste includes actions that do not contribute to patient safety or quality of care (and is not a regulatory requirement). Waste detracts from the time nurses and doctors have to provide safe and effective care.”
Written next to that, on the same dry-erase board, is a question: “What could have made your job easier today?” It is posed to all front-line staff as an opportunity to share what could be helpful and to call out what is wasteful.
When front-line staff identify barriers to the delivery of high-quality, efficient care, the Clinical Nurse Specialist (CNS) team — led by Kim Elgin, DNP, RN; Amy Johnston, RN; Dea Mahanes, DNP, RN; and Kathleen Rea, DNP, RN — connects them with leadership to find a solution. Since last fall, the CNS team has been on a mission to reduce or eliminate waste wherever it may be found.
When rounding with a multidisciplinary group in February, front-line staff identified an issue with our barcode scanners. All 617 of them.
What’s With the Barcode Scanners?
A CNS is an advanced practice provider who, in addition to providing advanced specialty care to patients, works to impact patient outcomes by partnering with nurses and within complex systems. Our CNS team connects organizational leaders with the front-line nurses to drive improvements. It was at this intersection where the CNS team found a way to fix the barcode scanners for front-line staff.
The barcode scanners are made of plastic and metal and electronics. Over time, they warp, get worn, or just degrade from daily use. As such, they do not always sit properly in their cradles for recharging. This directly impacts medication administration.
Johnston says, “In some instances, the scanner would have just enough charge to scan only one medication. The nurse would then have to put the scanner back on the charger and wait a few seconds before it was ready to scan again.”
Mahanes says, “Even if a glitchy scanner only adds 30 seconds to each med pass — that adds up over time. Replacing these scanners is going save time for our nurses and provide better safety for our patients.”
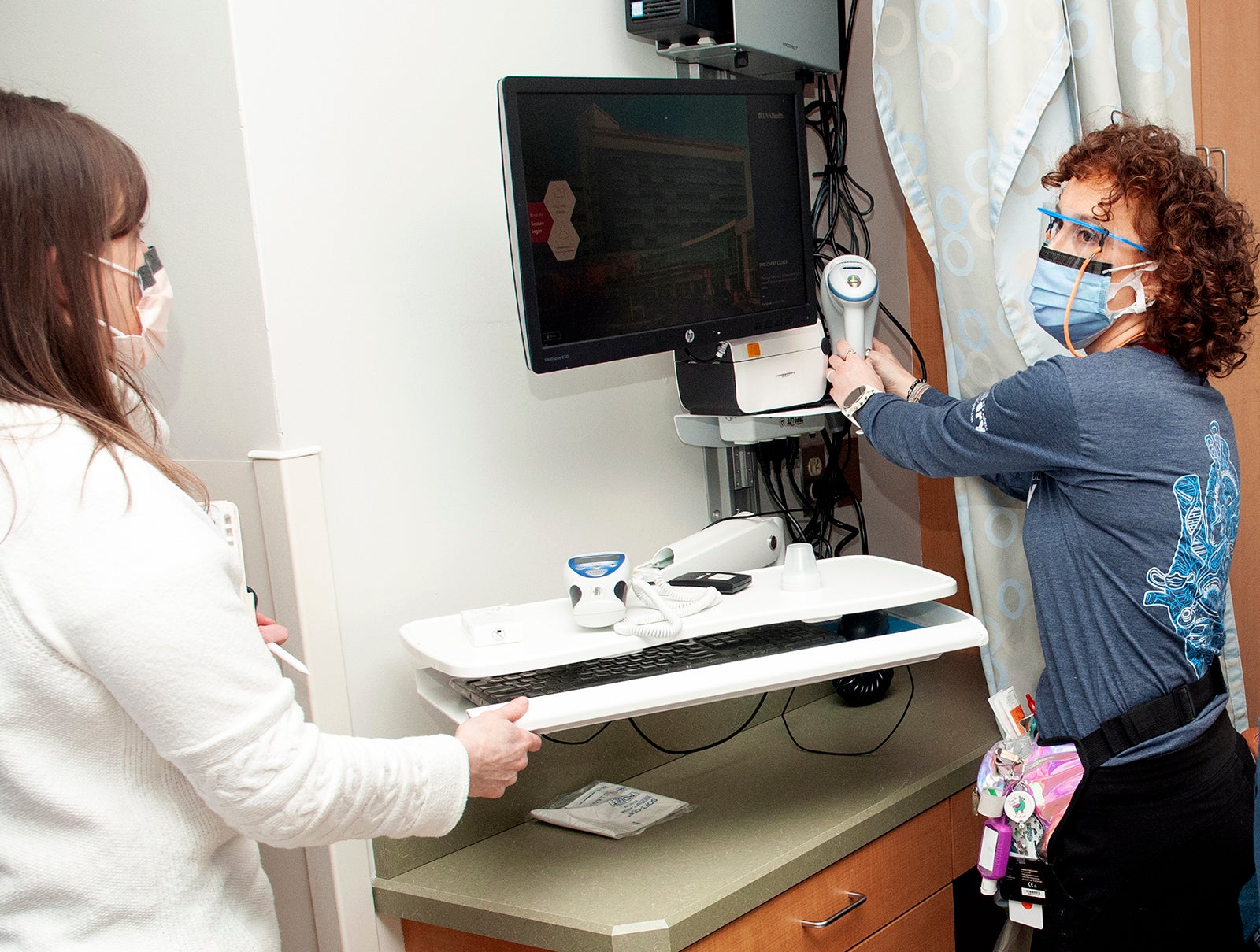
“Additionally,” says Elgin, “the current scanners are not placed in the room appropriately, in terms of being in an ergonomically safe place to reach.” In some rooms, nurses have to reach behind a curtain or around a monitor (or sometimes both!) to get to the barcode scanner. This is not ideal placement for a critical piece of equipment with a high rate of use.
The CNS team partnered with IT, facilities, and leadership to replace the 617 scanners as soon as possible. Elgin says a few have already been replaced on the fourth floor, but that the bulk of the new scanners will be installed in the coming months. “Team members will see firsthand the downstream impact of their engagement. They are the ones who identified this problem. Right now, we’re ensuring that the front-line staff input is at the forefront as the scanners are physically being placed. They’re showing us where they want the scanners. We want to make sure we get this right for them.”
Liz Winn, RN, 4 Central Cardiology, and Kim Staples, RN, 4 Central Transplant, were the two nurses who initially broached the barcode-scanner issue during rounds with Wendy Horton, CEO, UVA Medical Center, and Reid Adams, MD, Chief Medical Officer. Staples says, “Because we do the job, because we’re taking care of the patients and using the equipment every day, we were able to provide feedback and be a part of making this positive change happen. I was impressed by this. Being listened to makes me feel supported.”
Horton says that she is inspired by UVA Health’s front-line staff. “People take pride in what they help to create and what they help to solve,” she says. “I think the best ideas come from the bedside, and the nurses who take care of our patients know best what needs to be changed and what needs to be solved. We have some of the smartest ideas and the brightest minds closest to our patients. That’s great for the institution and great for the patient. We want everyone to be empowered to create the necessary change in the organization.” The barcode-scanner problem is just one such example of how front-line staff are affecting positive change.
Elgin says that, while there had already been a plan to replace the barcode scanners, it was contingent upon budget in the next fiscal year. “It wasn't planned as an immediate fix. It was coming down the road. But these scanners were either failing or would fail in the next year. They were at the end of their life cycle. When Wendy and Reid were made aware of the problem, they wanted to act. Wendy was rounding with us and she basically said, right then and there, ‘We need to figure out how to make this happen sooner.’”
Horton says, “When you see, for example, a transplant patient who needs more than 10 medications and the nurse is scanning each one and the scanner is not working properly … you multiply that times our number of patients and their medications and the number of times a day they need to take a medication… it compounds. And it's frustrating. You see front-line staff running around, trying different scanners or not using the scanner, which then creates a safety problem. People are trying their absolute best, but we want to make sure that everyone has the tools that they need. When you're there on the floor, standing next to the front-line teams, and seeing it in action: Making the decision to replace the scanners was a no-brainer.”
The Spark That Caught Like Wildfire
Mahanes credits Laura Polliard, RN, NNICU, with pointing out that, as UVA Health struggles with staffing — as most hospitals are across the country — anything that can be done to help nurses is a win. “She said, ‘If we can't find additional nurses immediately, what can we do to make the care we provide more efficient, so that we have more time to spend at the bedside?’ That was the idea and it has spread like wildfire.”
The CNS team is looking at multiple areas where they can reduce waste and frustrations for front-line staff, while increasing efficiency. They are partnering with five areas, which include Pharmacy, equipment, supplies, IT, and Nutrition Services. They are working locally with teams to address challenges at the unit level.
Mahanes says, “We want to find opportunities where we can provide better patient care. Everyone is engaged in getting feedback and ideas from staff. The 14 CNSs on our team have spoken with staff across inpatient areas and asked them what they thought the issues were. This empowered the bedside staff to raise awareness of problems — and then, hopefully, to engage in helping us find a solution together.”
Polliard says that, as a result of this work, the team has been or is currently investigating positive changes for staff and patients alike. “Things like rescheduling when computers reboot, upgrading the barcode scanners, troubleshooting issues with bladder scanner batteries, or providing nutritional needs or controlled substances for patients so nurses don’t need to leave the unit.”
Basically put: “What could have made your job easier today?”
Thank you to all involved in getting the barcode scanners replaced. From identifying the problem, to finding the money, to purchasing and installing the technology, to coordinating time when the patients are out of their rooms … this has been a real team effort. Congratulations (and a big thank you) go out to the CNS team, Otis Hackett and the facilities team, Richard Shelley and the IT team, leadership, and myriad unit nurses, assistant nurse managers, and nurse managers. Thank you!
Latest News








What a fantastic way to support nursing and show the front line team they are being heard! Well done and very inspiring!