
Discovery Reveals How Ketogenic Diet Prevents Seizures When Drugs Fail
University of Virginia School of Medicine researchers have revealed how the popular, low-carb ketogenic diet protects against epilepsy seizures and possibly neurodegenerative diseases such as Alzheimer’s and Parkinson’s.
Keto, as the diet is commonly known, has been used to reduce seizures in patients with medication-resistant epilepsy since the 1920s. Doctors, however, have been uncertain exactly how the diet does this, even as they identified potential benefits for other brain disorders.
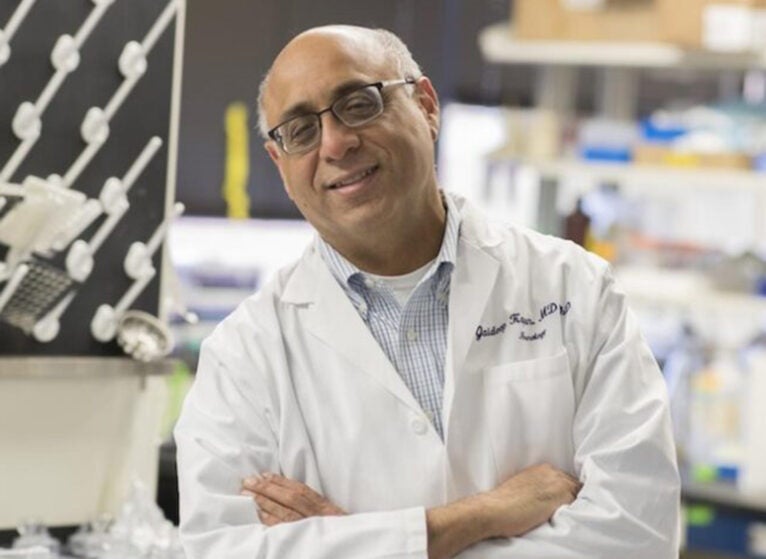
A team led by UVA’s Jaideep Kapur, MBBS, PhD, co-director of UVA’s Brain Institute, has found answers. This discovery could eventually allow patients to reap the benefits of the keto diet without the highly restrictive eating — almost devoid of sweet treats and comforting carbohydrates — necessary to stay “in keto.”
“The body converts the keto diet to a ketone body called β-hydroxybutyrate. We discovered that HCAR2 helps β-hydroxybutyrate reduce seizures by regulating the activity and communication of brain cells,” said Kapur, an epileptologist (epilepsy expert) at UVA Health and the School of Medicine’s Department of Neurology and Neuroscience. “Many individuals are unable to tolerate the keto diet due to high fat content and side effects. This discovery helps find drugs that have the beneficial effects of the keto diet. Niacin, an FDA-approved lipid-lowering drug, also works on HCAR2.”
Keto Diet Brain Benefits
The keto diet aims to encourage our bodies to burn fat instead of carbohydrates for fuel. This can provide obvious benefits for those trying to lose weight, but it also causes unseen changes in the body, and many people cannot tolerate such a high-fat diet. Keto prompts our livers to produce molecules called ketones (ketosis), which replace easily burned carbohydrates as fuel for our brain cells.
Kapur, researcher Soudabeh Naderi and their colleagues found that one of the most common of these ketones, β-hydroxybutyrate, interacts with a specific cellular receptor to reduce seizures in lab mice. It does this by calming nerve cells called neurons, the scientists found. When neurons become too excitable, they can trigger seizures. Hyperactive neurons are also seen in early Alzheimer’s and in other conditions, such as autism.
As part of their research, Kapur and his team mapped out the receptor’s presence in the hippocampus, the portion of the brain where seizures often begin. They found the receptor, hydroxycarboxylic acid receptor 2, was concentrated in a particular cell type already linked to seizures. The receptor was also common in immune cells called microglia that patrol and protect the brain.
The researchers’ work suggests that it may be possible to develop drugs to give patients the brain benefits of the ketogenic diet without being on the highly restrictive diet, which can come with unwanted side effects such as gastrointestinal distress. For example, the scientists’ early work in lab mice suggests that niacin — vitamin B3 — may provide at least some benefit, though more research would be needed to determine if this benefit holds true in people.
“We are now exploring how this receptor modulates brain immune responses through microglia,” Kapur said. “These studies would allow us to come up with novel therapies for drug-resistant epilepsy and potentially other disorders such as multiple sclerosis and Alzheimer’s disease.”
About UVA’s Cutting-Edge Brain Research
Finding better ways to treat epilepsy, Alzheimer’s, and other neurological diseases is a core mission of UVA’s new Paul and Diane Manning Institute of Biotechnology. That institute works together with UVA’s Brain Institute to bring top experts across UVA to speed up the transformation of basic scientific discoveries into new treatments and cures that will help patients across Virginia and around the world.
Kapur and his colleagues have published their new findings in the scientific journal Annals of Neurology. The research team consisted of Soudabeh Naderi, John Williamson, Huayu Sun, Suchitra Joshi, Rachel Jane Spera, Savaira Zaib, Supriya Sharma, Chengsan Sun, Andrey Brodovskiy, Ifrah Zawar, and Kapur. The scientists have no financial interest in the work.
The research was supported by the National Institute of Health’s National Institute of Neurological Disorders and Stroke, grants R01NS120945 and R37NS119012, and the UVA Brain Institute.
To keep up with the latest medical research news from UVA, bookmark the Making of Medicine blog.
Latest News



