Back-to-Basics Course Helps Students Step into Clinicals
Oh, they knew the course.
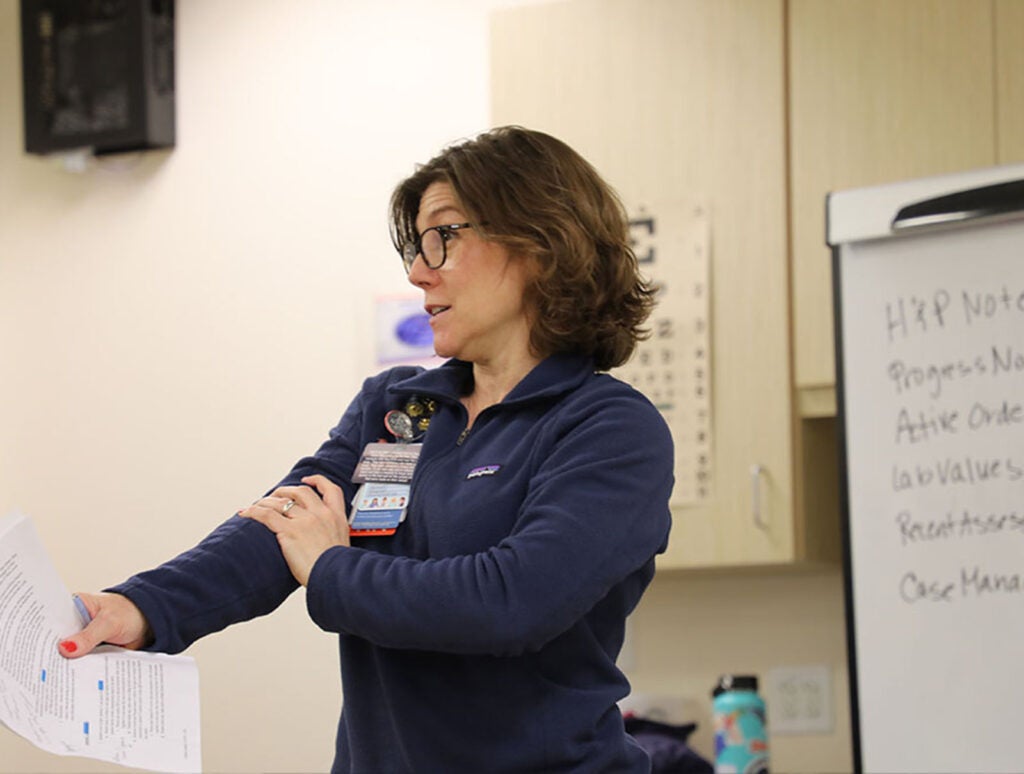
Clinical instructor Laurel Geis (MSN ’07) had taken a similar class while a nursing student, and Sarah Craig (MSN 10, PhD ’14), Associate Professor, had taught Case Based Learning (NUCO 2440) as a graduate teaching assistant while earning a doctorate.
As faculty, they’d even taught it together in 2024, and knew the class was positioned to help second-year nursing students tie together what they’d so-far learned as they began their first clinical rotations.
But, for many, the transition from classroom to clinicals was still rough. Some students got “stage fright” during patient encounters, became tongue-tied, hung back, or froze when confronted with a complex patient in the hospital. They hadn’t quite stitched the intellectual and clinical skills they’d so far amassed together, and the gaps often showed.
“It’s one thing to be great in the classroom as a nursing student,” said Craig, “but a whole different ballgame to perform, implement the knowledge you have, and fight against the imposter syndrome that many of us have early in our nursing education.”
The deficits weren’t because students were shy, afraid, or ill-suited for nursing, but because they hadn’t been well-prepared. Across its long life, the Case-Based Learning course had lost touch with many of its objectives, the result of clinical faculty teaching what they loved and were interested in, rather than the foundational skills that students needed to repeatedly learn and practice to ready them for the hospital setting.
“We weren’t hard wiring the basics,” Craig said — basics that are outlined in the American Association of Colleges of Nursing’s 2021 Essentials, a curricular compass that aims to close the kind of academic to clinical practice gaps Craig and Geis observed.
So Geis and Craig started by working backwards. What, they asked one another, were the skills students needed to possess by course’s end? And what new kinds of assignments and experiences would help get them there?
Charting. Bed-baths. How to introduce oneself to a patient. Foley care, moving someone from a bed to a chair, executing blood sugar tests. Yes, there’s a lot more to nursing, they knew, but they zeroed in, peeled away busy work, and came with a trifecta of new key signature assignments that provided students with the essential nursing skills they’d need to take a more confident step toward clinical care.
First up: A semester-long fundamental skills assessments checklist, which helped ensure they were competent and confident in basic skills they’ll need in future clinical rotations. A new simulation focused on how to chart in EPIC, UVA Health’s electronic medical records software. And a series of assigned reflective writings on everything from a script for how they’d introduce themselves to patients to their personal reflections on clinical rotation to several formal investigations into pathologies, topics like heart failure, gastro-intestinal disease, or stroke. By semester’s end, their writings, documentation of clinical hours, and skills checklists were tidily entered into their electronic TYPHON portfolios, where “they could reflect on their growth and show their progress,” Craig said.
Perhaps most importantly, though, was the course’s determined shift to ensure students’ active involvement in — not passive observations of — clinical care in their work on the units and with preceptors.
“We tell students, ‘You are not shadowing. It’s active care,’” said Geis. “‘It’s OK if you don’t know the answer to a patient's question,’ we say. ‘This is about building your confidence to be in the space.’”
“We flipped to developing confidence and clinical judgement as a primary objective,” added Craig, “versus task-oriented training, which helps students see the bigger picture of team-based patient care and the real role of nurses.”
While energized by their course overhaul, the duo got some push back from colleagues who felt they’d decreased the course’s rigor—a sentiment they politely but firmly refute.
“I don’t think what we did was make it easy,” Geis countered. “I think we made it less busy. I think it made us able to focus on helping these students become better nursing students, and to get the practice they need.”
As the course continues to evolve, it’s given Geis, Craig, and other faculty members a practical vision of Essentials and the competency-based education it champions. The process “helped me realize what competency-based education really is, seeing it in action versus in theory,” said Geis. “We didn’t go back in and redefine course objectives; we worked within those objectives to get back to the basics, some of which were getting lost in our old format.”
“This,” added Geis, “is what [the Case Based Learning course] 2440 is supposed to be.”
Latest News