Hope at Work: How a UVA Health Culpeper Medical Center Team Collaborates With Local EMS to Save Newborns
This is the latest installment in our Connect article series “Hope at Work” — showcasing inspiring stories about how our team members contribute to UVA Health’s 10-year strategic plan: “One Future Together Health and Hope for All.” No matter where you work, you have an opportunity to inspire hope in others. These stories show how:
Whether it’s a birth in the back of an ambulance, a home birth with a complicated outcome, or a parent finding their infant not breathing — emergency medical services (EMS) staff are the first medical professionals on the scene. Yet, training in neonatal resuscitation is not common for them.
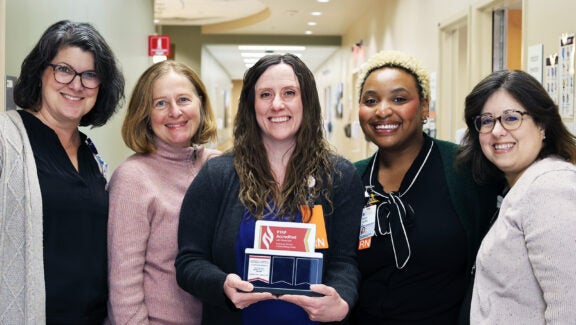
The only training available is through hospital programs, such as the one at UVA Health Culpeper Medical Center. The 70-bed, rural hospital recently reached out to local EMS providers and began training and partnering with them through their neonatal resuscitation program (NRP).
“Being NRP-certified will prepare EMS staff to provide the very best care in case of a neonatal emergency in our community,” says Michelle Curran, MSN, RN, CCRN, Clinical Nurse Educator, UVA Community Health, a team member involved in the initiative.
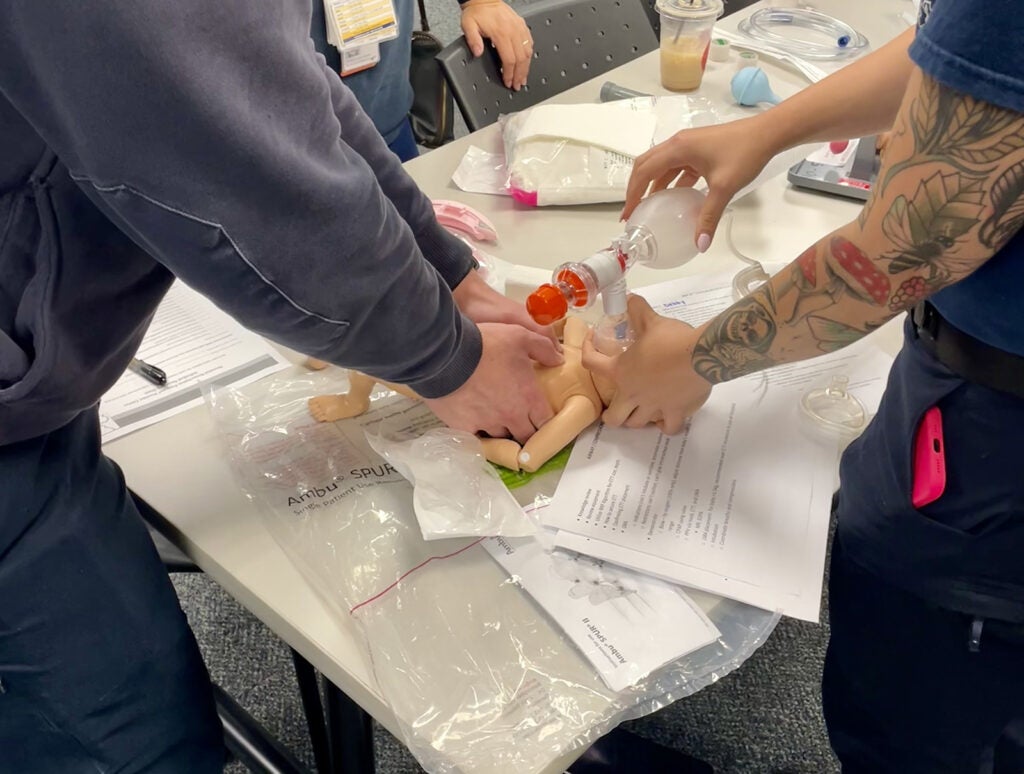
The NRP at UVA Health Culpeper Medical Center in partnership with the American Academy of Pediatrics (AAP) takes a rare approach to newborn care — addressing preparation for a birth, teamwork, and clinical skills with a focus on ventilation of the newborn.
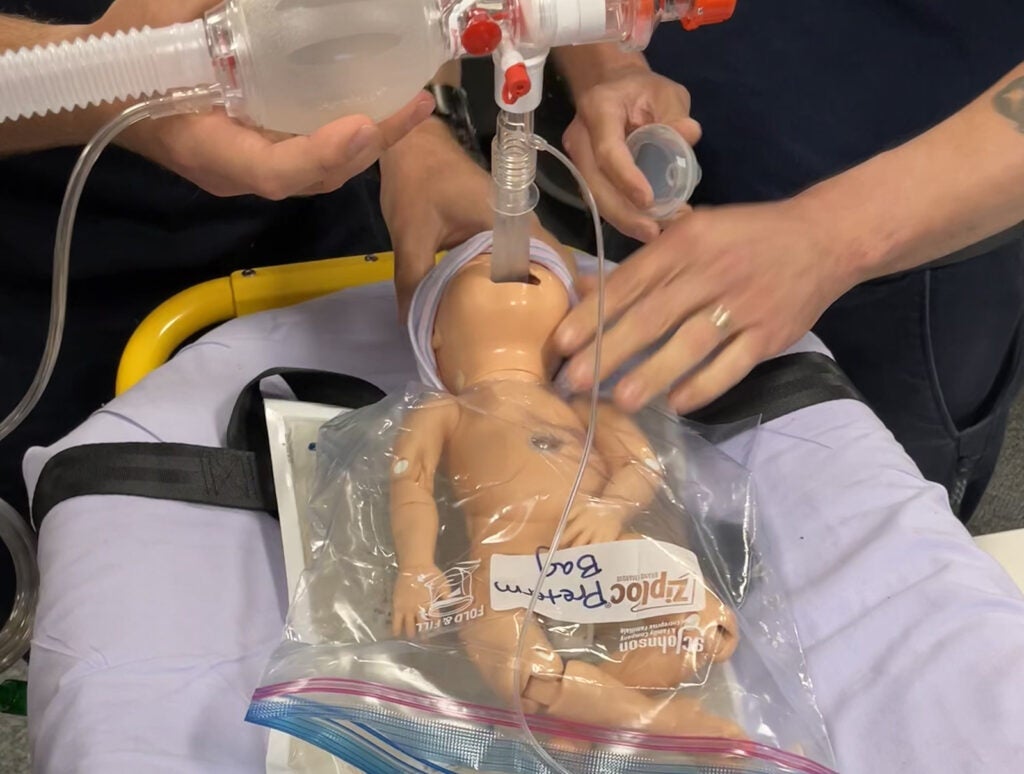
“As most clinicians know, in the adult patient world, the priority is high quality CPR [cardiopulmonary resuscitation]. With newborns, there’s generally nothing wrong with their hearts — if they are in distress, it is likely a ventilation or oxygenation issue. Also, understanding the importance of maintaining a normal temperature in a newborn can be lifesaving. This partnership is important because this training is hard to come by as it is typically only offered in hospital settings,” explains Michelle.
Perfect Match
Leah Pearson, BSN, RN, C-EFM (certified-electronic fetal monitoring), RNC-NIC (registered nurse certified-neonatal intensive care), who works at the Family Birth Center, UVA Health Culpeper Medical Center, met Jeremiah Halsey years ago when his children were born at UVA Health Culpeper Family Birth Center.
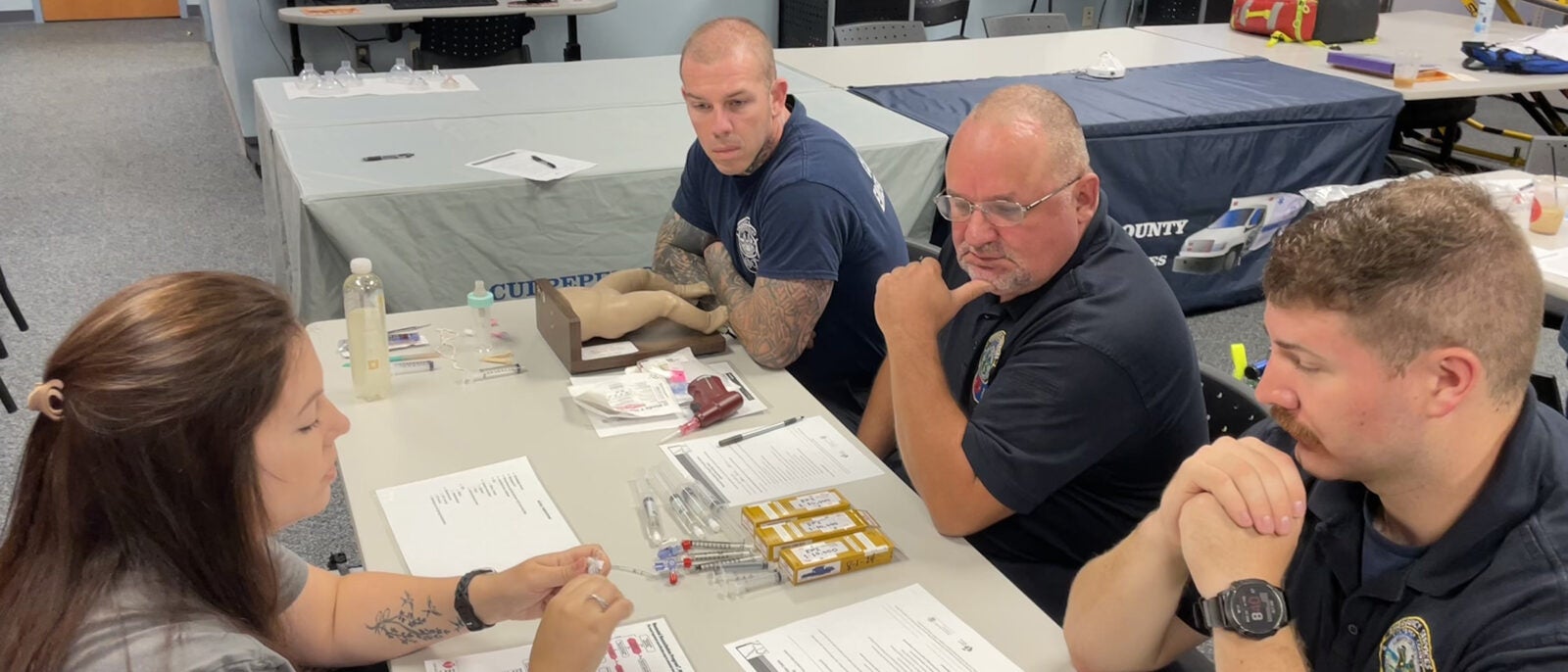
Now an emergency services technician (EMT) and lieutenant with Culpeper Office of Emergency Services, Jeremiah approached Leah in early 2024 about offering a NRP course to the career EMS staff. “I believe training develops competence and competence manifests in confidence. We are professionals and we want to give the absolute best care to all our patients, especially the new arrivals.”
“He and his coworkers, including my paramedic husband, recognized the need for newborn resuscitation as a rare but high acuity event that they wanted to learn more about and become more proficient in managing,” Leah says. She was asked to talk to Michelle because she's the NRP program facilitator.
Leah, a UVA School of Nursing alum, completed an externship in UVA Health Neonatal Intensive Care Unit (NICU) where she says she met incredible nurses and fell in love with newborn care. After graduation, she worked as an RN in the NICU until 2017.
After moving to the Culpeper area, she took a position with UVA Health Culpeper Medical Center in 2017, where she was encouraged to become an NRP instructor because of her background.
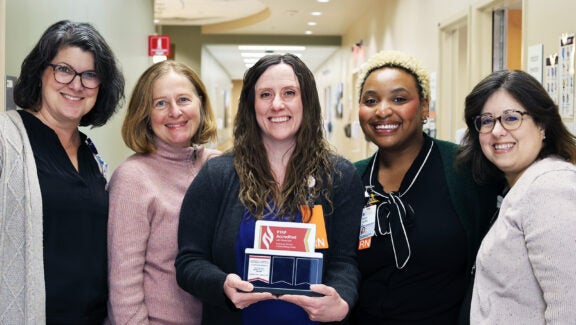
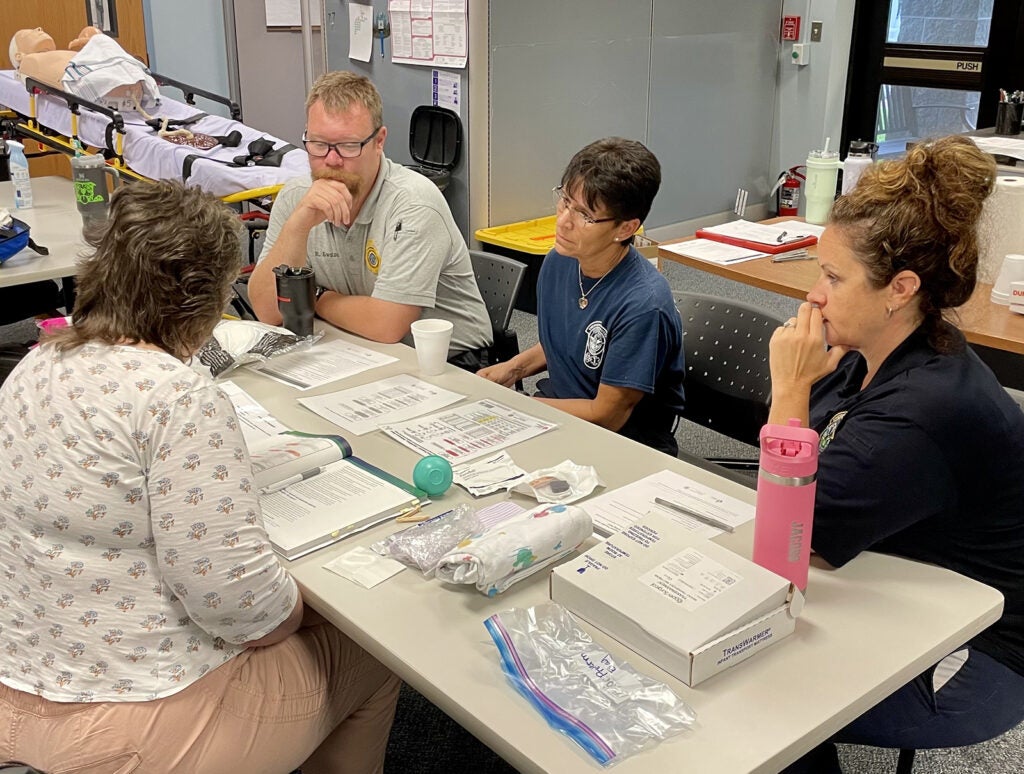
“For several years, I’ve been able to teach NRP alongside our unit’s other NRP instructors: Dana Demers and Debby Carver. We offer the class to interdisciplinary staff, including nurses, respiratory therapists, and pediatricians. Newborn care remains a passion of mine and I’m so proud to work with top-notch staff. It made sense to extend this resuscitation education to the out-of-hospital providers who service the same community that my unit serves,” says Leah.
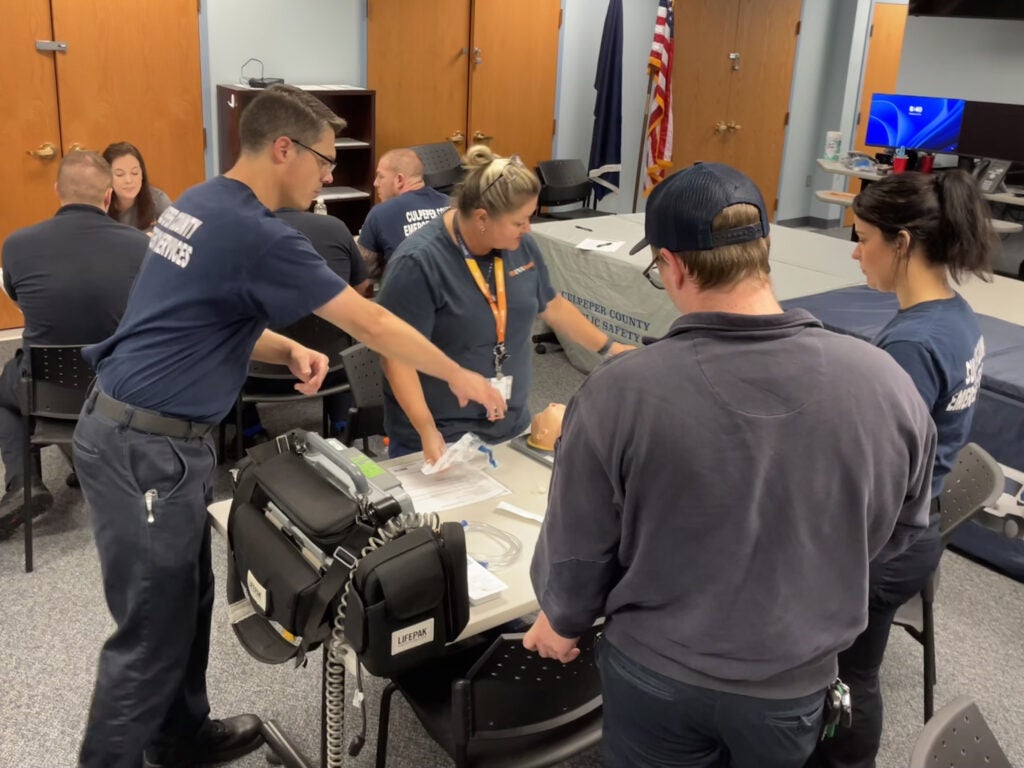
She was wholeheartedly on board and more than qualified to help create this partnership and agreed to teach the course with Dana and Debby on a volunteer basis. Jeremiah presented this idea to the director of the Culpeper Office of Emergency Services (COES), who also supported it and agreed to take on the cost of the online portion of the NRP program required to be completed before the in-person course.
It All Comes Together
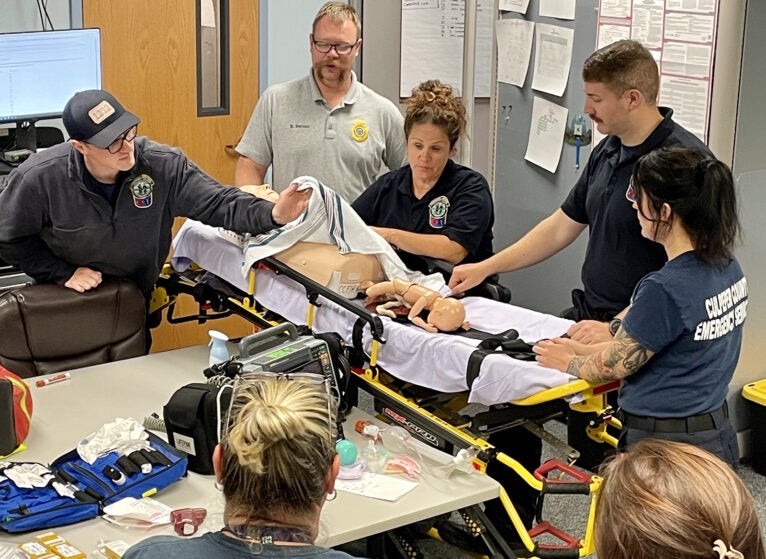
Michelle and Matthew P. Rhames, MD, gave Leah and Jeremiah guidance about the scope for EMS providers in terms of what interventions could realistically be accomplished outside the hospital and brought a focus to thermoregulation as a priority for the newborn, and how EMS would manage this.
“In the hospital environment, skin-to-skin contact between a newborn and mother is a key to keeping a baby warm (mother holding bare baby against bare chest). In the ambulance, the newborn needs to be buckled in, so skin-to-skin contact is not possible. If Mom also needs care, she must go in another ambulance, " Michelle says.
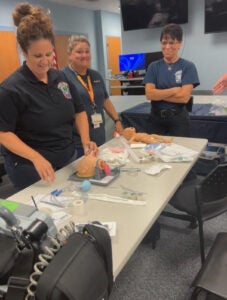
“We've made some suggestions about practices and integrating products such as a thermal mattress that likely will be put into effect soon,” Leah says.
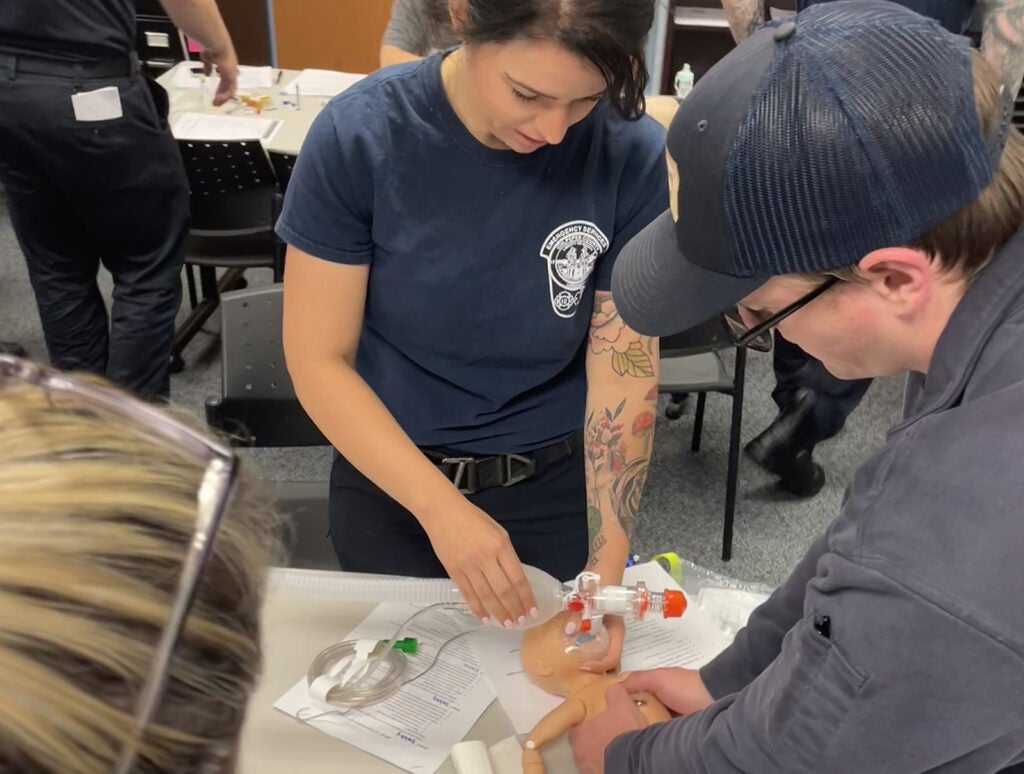
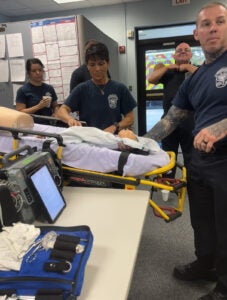
Over the last few months, Leah has made a few visits to the EMS station to learn about processes they currently have in place, the supplies the ambulance is equipped with, and possible barriers. She also worked with Dr. Rhames., who offered guidance on the NRP skills the EMS providers can perform, including preferred methods for IV access and alternative airways for EMS providers, so that Leah could incorporate them into skills stations.
Leah explains she’s modified the class compared to what she teaches in the hospital class. The class in the hospital goes over setting up the specific equipment they use and how to call for more help and extra hands. She tailored this new class to the environment that the emergency would be occurring in — someone’s home or in the back of ambulance — and used only the equipment that these out-of-hospital providers would have on hand.
The teacher is not the only person with challenges. Explains Jeremiah: "NRP is vastly different from the motor memory that EMS professionals develop in their practices of CPR, ACLS (advanced cardiovascular life support), and PALS (pediatric advanced life support).”
Onward and Upward
“The qualitative feedback is positive," Leah reports.
"I believe we achieved the goal set forth and those who participated are more competent in caring for neonates,” adds Jeremiah.
They plan to continue the program indefinitely and will schedule the class annually for both newcomers to the program as well as every two-year recertification that is required by NRP.
Jeremiah points out one of the greatest benefits to this partnership: the instructors were forward thinking, willing to come to them, and helped them to develop best practices using the equipment they carry and make recommendations on the equipment they should be carrying.
“My coworkers and I may be receiving these babies for admission after transport, and my hope is that they will be stable and warm upon arrival!” says Leah.
Latest News