From left: Robert Goldstein, MD; Anne Croonquist, RN; Dania Chastain, PhD; Wendy Carlton; and and Virginia Leavall, Chief EMS, Albemarle County Fire and Rescue and Hazardous Area Response Team (HART) Specialist.
Hope at Work: How UVA Health Team Members ‘Educate, Empower, Connect’ During Pain Awareness Month — and Year-Round
This is the latest installment in our Connect article series “Hope at Work” — showcasing inspiring stories about how our team members contribute to UVA Health’s 10-year strategic plan: “One Future Together Health and Hope for All.” No matter where you work, you have an opportunity to inspire hope in others. These stories show how. September is Pain Awareness Month:
Dania Chastain, PhD, and Anne Croonquist, RN, are on a mission.
Dania — Associate Professor of Clinical Anesthesiology, UVA School of Medicine, and Founder and Director, Office of Pain Management and Opioid Stewardship (OPMOS) — inspired to fill a dangerous void.
Anne — a nurse of nearly 40 years — motivated by a tragic loss.
One Pill Can Kill
Anne has taken care of countless patients ranging from pediatric to geriatric to hospice. In 2013, she became an Albemarle County, Virginia middle school nurse to accommodate the busy schedules of her four children. When the COVID-19 pandemic took hold in spring 2020, she joined UVA Health to work in Physical Medicine and Rehabilitation, in addition to supporting Spine Care and Pain Management.
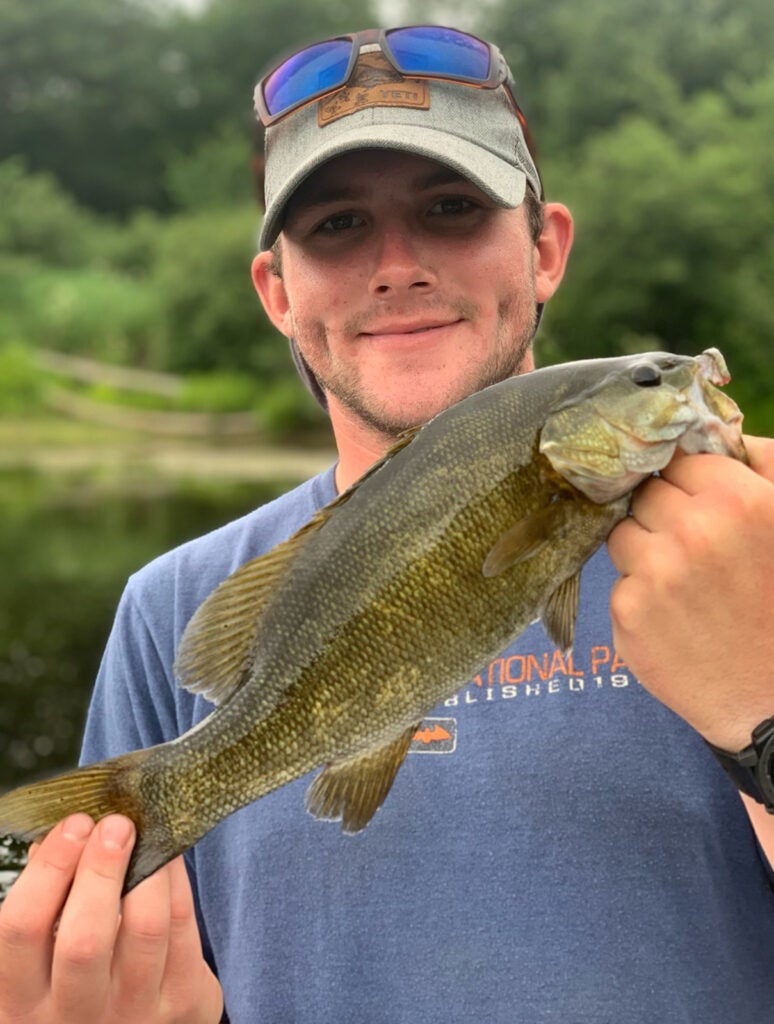
On June 3, 2022, the nurse who’d dedicated her career to helping others, came home and felt helpless — shocked to find her 23-year-old son had passed away on the couch a few hours prior.
“Kevin had the kindest spirit. He loved anything outdoors and was such a hard worker. He was not someone who used drugs on a regular basis. But on this particular day, he had been dealing with some depression and some anxiety,” recalls Anne. “On this day, he decided to self-medicate in hopes that it might make him feel better. So he connected with someone through social media, then used a mobile payment app to pay for some pills. They met next to a fast food restaurant right here in Charlottesville.”
Anne says Kevin bought a few pills and took one — that one pill turned out to be laced with illicit fentanyl.
“And there was enough illicit fentanyl in that one pill to kill him,” she describes.
'Not in Vain'
In 2024, Anne turned grief into action and reached out to the local board of education, superintendent, and principal. Then, the head of nursing at Albemarle County Public Schools introduced Anne to Dania, who offered to Anne an opportunity to speak at OPMOS events through the community. When Anne’s children encouraged her to share Kevin’s story, she agreed: “I always promised myself his death would not be in vain,” she says determinedly.
Every time Anne goes public with Kevin’s story, it takes a few days for her to recover from recounting the devastating loss. “But even if only one child in the audience listens to me, it’s worth it,” she insists.
Adds Dania: “The courage that it must take for Anne to share her story — the teachers and students embrace her — you can hear a pin drop. She does a really amazing job! It’s such a gift she’s giving to all of us.”
‘The Very First Time’
Dania — a board-certified, leading clinical psychologist specializing in pain management and opioid stewardship — says when certain non-opioid drugs are being mixed with fentanyl, in some cases, the resulting combinations are exponentially more dangerous and can’t be reversed by Narcan, the brand name for naloxone — a lifesaving medication that can reverse the effects of an opioid overdose.
“We’re trying to stay a step ahead,” says Dania, “but sometimes, the dealers are ten steps ahead. We’re seeing new drugs — such as N-methylclonazepam, a benzodiazepine derivative, and nitazines, which are synthetically engineered to mimic effects of traditional opioids — mixed with fentanyl.”
Dania emphasizes: “No one is looking for or expects they would be getting counterfeit pills. Fewer than 5% of overdoses are suicides. Most people are curious, partying, or trying to get through a rough time. They think they’re getting an Adderall to help them stay up and study for an exam, or they think they’re getting a Xanax to feel more comfortable socializing — but it may be a counterfeit pill containing fentanyl. For so many young people, alarmingly, the very first time they try anything, they may be getting a counterfeit pill!”
Stunning Statistics
OPMOS and its events are a result of Dania’s drive to sound the alarm in our area about the opioid crisis. She recounts the horror of a new reality emerging in communities across the country even before the COVID-19 pandemic: fentanyl overdose death rates skyrocketed 657% from 2014 to 2019 — reaching 36,400 by the end of 2019.
When the lockdown hit in spring 2020 — Dania says more people used opioids in isolation, and patients living with pain were afraid of becoming addicted, so instead of reaching out for help, they suffered in silence. Anxiety and depression increased as they became separated from mental health services, friends, and families — and left in a vulnerable position.
The pandemic eased by 2023, but fentanyl overdose death rates soared to 72,899.
“And as we emerged from the pandemic, once again we saw our landscape changing,” describes Dania. “Now — fentanyl, fentanyl derivatives, counterfeit pills, and illegal online pharmacies pose exceptional threats! The face of those who overdose also has changed.”
Transforming Health and Inspiring Hope
Dania couldn’t sit on the sidelines. She founded OPMOS in 2020 with the goal of establishing and fostering interdisciplinary, collaborative educational pain management initiatives within the University and the health system — and in partnership with the local community and national partners. The focus: communication, treatment, collaboration, safety, and empowerment.
She says the resulting research shows that the opioid crisis changed the way we evaluate, treat, and anaylze the field of medicine in general — and pain management, specifically.
“It’s our UVA Health mission to transform health and inspire hope,” she points out. “We had not tackled a problem like this before, but we felt a sense of responsibility. Providing education is a great way to give back to our community.”
Since then, OPMOS has provided individualized programming, honing in on research-based best practices across the medical community — offering pain management and opioid-informed training to non-pain trained providers, nonprofits, patients and families, students, and parents.
“I am grateful that my department, Anesthesiology, recognized the value of OPMOS and graciously supported this initiative from the onset,” says Dania. “We have such talented pain management attendings; together, we provide the backbone and expertise. Having Wendy Carlton as our Program Director also has been beneficial to the growth of our programs and outreach. In addition, our interdisciplinary advisory board brings rich and unique perspectives to the table.”
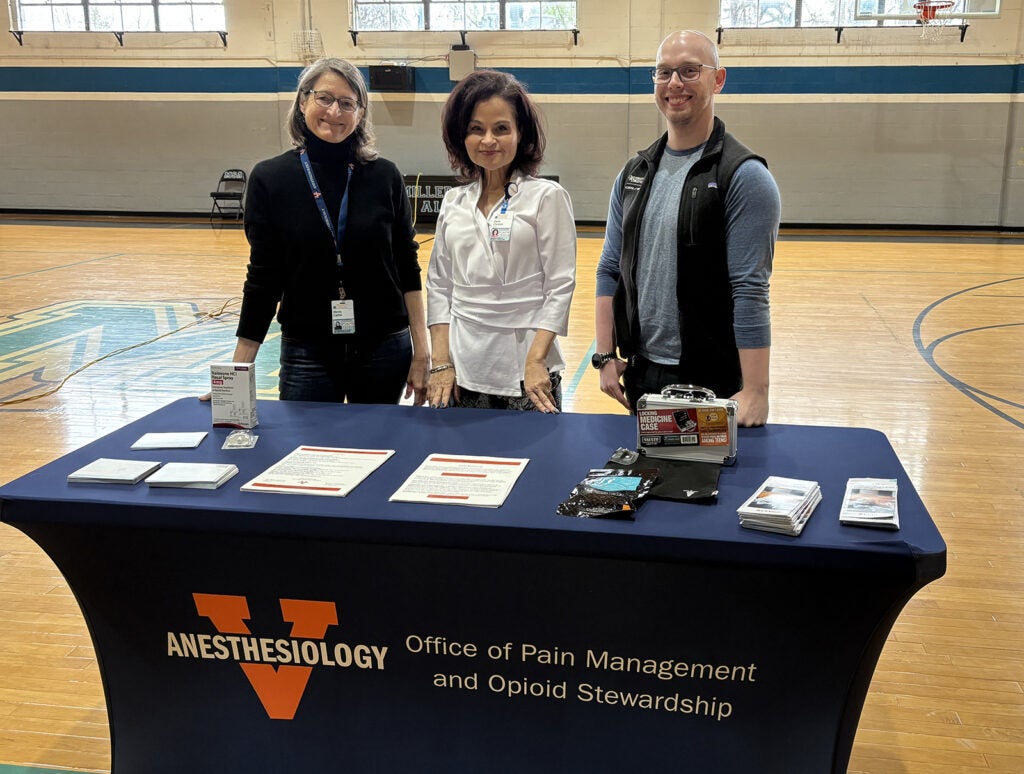
Drug Take Back Day
Among the safety initiatives: each year, the Department of Anesthesiology and OPMOS — in partnership with UVA Health Pharmacy and UVA Police — plan a community Drug Take Back Day. The fall 2025 event will be held Saturday, Oct. 25, 10 a.m.–2 p.m., outside Emily Couric Clinical Cancer Center, 1240 Lee Street, Charlottesville.
Educating and Empowering the Next Generation
NPR reports the latest available records show fentanyl and other drugs killed more than 31,000 people under the age of 35 in 2021. By 2024, that number had plummeted to roughly 16,690 fatal overdoses, according to provisional CDC data. But for those born 2005-11, considered to be among Gen Z, a slight uptick in deaths was reported in the past two years.
So OPMOS isn’t resting. In another initiative, UVA Health interdisciplinary team members visit area public and private middle and high schools, Piedmont Virginia Community College (PVCC), and UVA to educate, empower, and connect the next generation — and teachers, faculty, administrators, and staff — on:
- How opioids work, drug exposures, and use among young adults.
- The impact of fentanyl, xylazine, medetomidine, and counterfeit pills.
- Awareness of novel drugs mixed with fentanyl.
- How to recognize and understand substance use and abuse.
- Narcan training and Good Samaritan Laws.
- How to identify and stop overdoses.
- Being an “active bystander,” harm reduction, and supporting friends and family.
- Illegal online pharmacies, and medication safety and disposal.
“It's incredibly rewarding to go into the schools,” says Dania. “The first thing we usually ask is, ‘Have any of you been affected by the opioid crisis in some way?”
She becomes emotional sharing the responses: “Multiple people raise their hands and explain how it’s impacted them — no matter the socioeconomics, gender, age — the opioid crisis doesn’t discriminate. It has ripped families and communities apart!”
Lifesaving Measures
OPMOS has developed Continuing Medical Education (CME) programs on topics ranging from assessment — to pharmacological, nonpharmacological, minimally invasive procedures and surgeries to treat pain. The importance of interdisciplinary care, especially regarding mental health issues, is key. Safe opioid prescribing and alternatives are addressed. Also, wellness and warning signs of substance abuse for healthcare providers is a frequently requested talk.
At OPMOS programs, community partners Region Ten Community Services Board and Charlottesville Albemarle Rescue Squad have distributed Narcan and trained more 2,000 people on how to administer the drug.
What’s Next?
On Sept. 26, 2025 during UVA Homecoming Weekend and in cooperation with the UVA Medical Alumni Association — Dania, along with UVA Health anesthesiologist Lynn Kohan, MD, Medical Director, UVA Pain Management Division, and Director, Pain Fellowship Program — will talk about the long-term effects of chronic opioid use, as well as treatment with buprenorphine. The other sessions in the series on Nov. 13, 2025 and Jan. 15, 2026, will be virtual. UVA Department of Anesthesiology will provide free CE credit for participants.
This fall, OPMOS also is scheduled to teach PVCC students about the new realities of synthetic opioids and counterfeit pills. In addition, OPMOS is collaborating on a pain management program series for student veterans addressing specific treatments to assist with managing pain associated with the military service.
Seek and Share
OPMOS invites inquiries from individuals and organizations about educational events tailored to your needs. And if you’re a provider with pain management or opioid issues in your practice, OPMOS will collaborate on solutions.
“We also want to hear what is working,” says Dania. “If you’ve had success with treatments or initiatives, please share your wisdom and experiences with OPMOS at OPMOS@uvahealth.org or Program Director Wendy Carlton at wlc4a@uvahealth.org.
Latest News