‘Keep Talking’: Q&A With Nurse Scientist Randy Jones on President Biden’s Prostate Cancer Journey
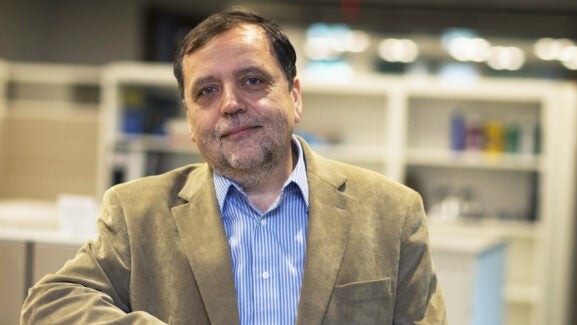
UVA School of Nursing Associate Dean and Nurse Scientist Randy Jones, PhD, RN, FAAN, FADLN, earned a $2.2 million National Institutes of Health (NIH) grant in 2017 to create, test, and deploy a decision tool to guide men with prostate and their family caregivers through treatment decision making — work he continues to refine for other treatment domains, too, like breast cancer.
When Jones first heard President Joe Biden was diagnosed with a previously undetected and aggressive form of prostate cancer — a disease process that’s usually slow growing — it reminded him that even presidents benefit from tools such as the one he created to guide frank conversations about treatment side effects as the former president navigates his cancer treatment.
When you first heard of President Biden’s stage IV cancer, what was the first thing you thought?
I was first concerned about how he was coping, along with his family members, about receiving the diagnosis when he hadn’t had any signs or symptoms of disease. I thought, “Wow. What’s he thinking? How’s he feeling about it all?”
It also reminded me that, being the former president, he had access to some of the best healthcare providers out there, and the cancer was still missed. What about the men who have few resources, and are limited in their health education? Individuals who don’t get routine medical care — maybe because they lack transportation, or come from lower socio-economic means, or can’t take off work to get to appointments or are un- or under-employed and don’t have insurance? There’s a lot of inequity in our system, but even so, the president’s cancer somehow got missed.
Prostate cancer is often a slow growing disease, though not always. It’s often recommended that men get screened for it starting around 40 if they’re at high risk. People at high risk either have a first degree relative, like a brother or a father who had prostate cancer in the past, but Black and African American men are also at higher risk. For those who aren’t in those categories, we usually recommend that people get screened with a PSA blood test starting at around age 45.
President Biden has been quoted in the media saying he’s “only taking a pill,” and that he “fully expects to beat the cancer.” What kind of treatment is he likely receiving and what things, especially in these early days, do you think he should know?
We don’t know the full story, so I don’t want to speculate too much, but he might be taking a treatment aimed at lowering the testosterone level in his body so it doesn’t produce more of what the cancer thrives on. Side effects for this kind of hormone therapy might include things like chest pain or heart palpitations, hot flashes, swelling of the prostate, or even allergies. When you’re dealing with hormones, those are the side effects that might occur. As is true with any treatment, I would advise him to share with his provider anything he experiences, even if it’s uncomfortable to talk about.
Would your decision tool for prostate cancer treatment decision making help President Biden at this point?
The tool I created is a conversation guide, really. We developed it to help patients and caregivers and their clinicians have more clarity as they make decisions about their course of treatment, but also as they start, change, or stop anti-cancer treatment, too. I’d think the tool would help the former president have a more open discussion of the pros and cons as he begins treatment. It could help his wife, Jill, as well as the clinicians treating him to talk so they’re all on the same page and can plot a path forward. Our tool helps lower decisional regret and increase quality of life.
When someone has prostate cancer, a lot of things change in their lives. But many people feel hesitant discussing the issues they’re facing with treatment, mostly because there’s a lot of stigma. Prostate cancer treatments affect men’s capacity: they might have erectile dysfunction, might become incontinent, they might feel like their role in their family may change, or that a partner or spouse might look at them differently. They may fear talking openly. The decision tool guides these conversations. People have a model to use to talk, kind of like a conversation “map,” and, using it, become more engaged, having a language to address their concerns. Regardless of what ultimately happens to them, the tool makes them feel that they gave it their best and we’ve found they have a lot less regret.
Why does that matter?
When people have high regret, especially at the end of their lives, it impacts them emotionally and mentally. They might say, “If I could have done this, maybe it wouldn’t have been so bad.” People with a lot of treatment-regret feel down on themselves, and that impacts of course, those around them, who wish they could have done more.
The decision tool helps us formulate the conversations we need to have. It’s hard for people to talk about prostate cancer side effects because they’re embarrassing: we’re ashamed that we can’t have sex easily, or at all; that we might be dribbling urine accidentally; that our loved ones might see us as weak; and that our roles in our families might change.
I remember one couple I worked with who used the tool — and who had more open conversations about prostate cancer and treatment side effects early on — said the tool was like having marriage counseling. They felt it made them closer. “I realized my husband was having all these difficulties,” the wife told me. “I heard what he had to say and understood better what he was going through even though he was embarrassed about the issue.”
That’s always stuck in my mind. People may have been partners for a long time, like President and Mrs. Biden have been, but certain topics can still have a lot of stigma. We still want to hide things because we don’t know how the other person will react. Open communication is such an important thing; it cannot be minimized.
What advice do you have for President Biden as he navigates treatment in these early days?
Keep talking. Speak candidly with your healthcare provider and continue to seek care as much as possible. Also, know you’re not alone in facing this kind of situation. If it’s helpful, find support systems and groups that might help you talk about certain issues in a comfortable, maybe still confidential way.
I’d also remind those around President Biden that we can’t put the onus on the patient to divulge everything. We healthcare providers need to make sure our patients with prostate cancer feel comfortable and welcomed in the healthcare environment and are able to answer our questions honestly and openly. We can use decision tools like the one I developed — which help us speak plainly with patients, avoid medical jargon, and then ask personal — sometimes difficult — questions matter-of-factly to open the conversation.
In nursing, we talk a lot about how to build quick rapport. Maybe we speak privately with the patient and then invite the spouse back into the room, because patients often say, “I can’t ask my wife to leave the room. That makes it more complicated! They’re my ride home.”
There are lots of different ways we clinicians need to really think carefully about how we interact with these patients, and how we build trust.
While not yet commercially available, Jones’ decision-making tool for prostate cancer is available for free through the NIH website. Reach Jones via email for more information.
Latest News