

Teamwork and Trust: Enhanced Communication Between Nurses and Technicians Improves Cardiac Monitoring Across UVA Health
Keeping patients with cardiac arrhythmias safe is a team effort. At UVA Health, part of that team is about a dozen miles north of University Medical Center, at the Central Cardiac Monitoring Unit (CCMU) in North Fork Research Park. From there, CCMU technicians monitor patients who require cardiac monitoring, pulse oximetry, and capnography. They support patients in the Emergency Department (ED), certain surgical admission areas, Cardiac Transition Unit, and both adult and pediatric acute and intermediate care units.
CCMU technicians are specially trained and certified in rhythm interpretation and monitoring, making them experts in cardiac monitoring systems. But patient safety, a key initiative of our UVA Health strategic plan and Nursing strategic plan, is about more than just technical skill. It depends on strong teamwork between CCMU technicians and bedside nurses — built on clear communication, shared understanding, and mutual respect.
Growing Risk of Alarm Fatigue
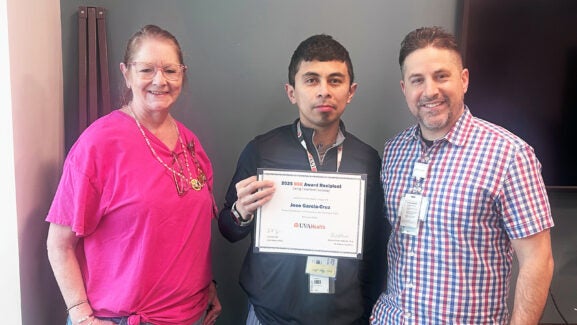
That teamwork became even more important in the fall 2025 when CCMU staff, bedside nurses, and nurse leaders came together to improve the care of patients requiring cardiac monitoring. “A key element of that work was the nurse-to-technician interface between the CCMU technicians and the bedside nurses in adult acute and intermediate care,” recalls Kathleen Rea, DNP, APRN, ACNS-BC, PCCN, CNL, Clinical Nurse Specialist, Adult Acute and Progressive Care (pictured above, left).
When the team sat down to examine CCMU escalation data together, an important trend emerged. During a one-week review period, only about one-quarter of CCMU escalations were related to true clinical changes. A significant portion (33%) of calls from technicians to nurses stemmed from non-clinical issues including loose or failed leads, oxygen saturation probes not attached or producing poor signals, low batteries, and missing or incorrect monitoring orders.
These issues, while not immediately life-threatening, were creating frequent interruptions and increasing the risk that meaningful alarms could be overlooked. “Looking at the CCMU data helped bedside nurses and leaders to appreciate that we were at risk for serious alarm fatigue,” explains Rea.
In response, the team launched a series of continuous process improvement steps to reduce unnecessary alarms. What emerged is a solution rooted in teamwork and trust, centered on improving communication between CCMU technicians and nurses.
The Verbal Check-In: A Simple Yet Effective Tactic
Rather than adding new technology or workflows, the team decided to introduce a verbal check-in at the start of each shift, giving charge nurses and CCMU technicians a dedicated moment to review and confirm cardiac monitoring orders. The benefits were immediate: orders were fixed right away, false alarms became less frequent, and communication improved. Just as important, team relationships grew stronger.
“Calling CCMU at the beginning of the shift has given me and the bedside nurses peace of mind, verifying that every patient who needs to be monitored is being monitored,” says Alli Kittrell, BSN, RN, CMSRN, Inpatient Charge Nurse, 5 West. “It also has allowed us to form, maintain, and build on interpersonal relationships with our CCMU team members. This process has improved patient flow hospitalwide by allowing 5 West to accept patients with monitoring orders from PACU [Post-Anesthesia Care Unit], ED, 5 North, STICU [Surgical Trauma Intensive Care Unit], and direct admits.”
“It feels collaborative and supportive,” adds CCMU Technician Karen Zitz, ECG-BC (pictured above, right). “Touching base with the charge nurse at the start of the shift gives us clarity about which patients need to be monitored — and why.”
Taking Action
Although still in its early stages, verbal check-in already has helped rebuild knowledge and skills in cardiac monitoring and strengthened communication between CCMU and nursing. Teams are reinforcing practical strategies such as changing leads more frequently, predicting when alarms might go off, and fixing equipment problems before they trigger alerts.
“We're really taking action to own our practice so that we get the benefit of the technology's help for our patients without the noise that can be so overwhelming,” describes Rea. “I love that we are tackling some of the hard details to reduce alarm fatigue!”
Latest News




As a Cardiac Monitor Technician at the CCMU, communication and understanding of both our protocols as techs, and the protocol of the RN’s we work with, is key to supporting patient safety. 5 and 3 West have been exceptional in their communication and updates throughout our shifts. As we are not on the unit with the patient’s we’re monitoring, there is a large gap in knowledge that only the RN’s working with them can fill for us. Remember, that there are people on the other end of the Vocera messages and phone calls- and we aren’t just ‘CMU #’ 🙂