
‘We Want Lifers’: New and Improved UVA Health Central Clinical Orientation
While strategic planning in 2020, UVA Health nursing leadership set a goal to evaluate and update the clinical onboarding program that had been in place for years. They knew welcoming new staff with a better quality orientation would make a significant impact on team members’ experience and retention and felt an overhaul was in order.
And now, after months of collaboration between Nursing Professional Development Services and UVA School of Nursing, a new approach to onboarding is live! Launched June 10, 2024, Central Clinical Orientation welcomes team members from across the spectrum of clinical care to UVA Health every other week, for two weeks. Connect spoke with several members of the team that made this new onboarding program a reality.
Q: Can you share some background on how this improvement project came to life and who was involved?
Mary Coffey, PhD, MPH, RN, NEA-BC, TIPC, Director, Nursing Professional Development: UVA Health University Medical Center Chief Nursing Officer Kathy Baker, PhD, RN, NE-BC, tasked a team of us to look at onboarding across the whole continuum and system and start to make a plan for how to improve. Since this is the work of welcoming our newest colleagues to nursing and clinical care delivery, we formed four teams that involved 55 people.
We knew our methods for onboarding had shifted since the pandemic. It was time to inventory what we were doing and find key opportunities for improving. Thankfully, there were great partners across the medical center and school of nursing working with me and Sarah Shreckhise, MSN, RN, Director, Ambulatory Clinical Professional Development.
By January 2024, it really took off. Joining our efforts were UVA Health University Medical Center Associate Chief Nursing Officer Karin Skeen, PhD, RN, NEA-BC; UVA School of Nursing Clinical Assistant Professor Kathleen Rea, DNP, RN, ACNS-BC, PCCN, CNL, Clinical Nurse Specialist Lead; other clinical nurse leaders; health system; IT and Human Resources colleagues — basically, anyone who touched the success of someone onboarding came to the table. I also oversee a team of 11 nursing professional development specialists who work closely with nurse managers, nursing education coordinators, and other staff members —it’s been a team effort for sure!
Q: What are its basic components?
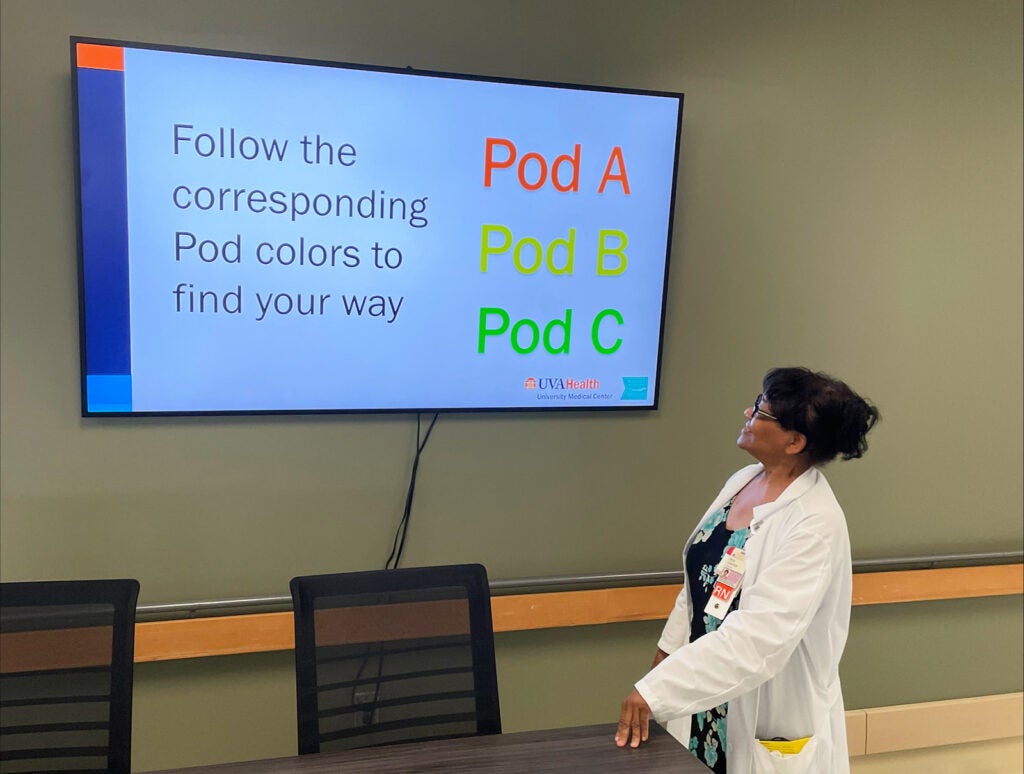
Shreckhise: We have expanded the orientation to include all clinical team members — from CNAs, patient care techs, and medical assistants to LPNs and RNs. In addition to including all clinical roles, it was also expanded to be inclusive of ambulatory.
Drew Ellen Gogian, EdD, MSN, RN, Nursing Professional Development Specialist-Lead: I think it’s great UVA Health Children's has joined us in this work. They will have their own specific orientation day when they validate their skills that are specific to Children’s.
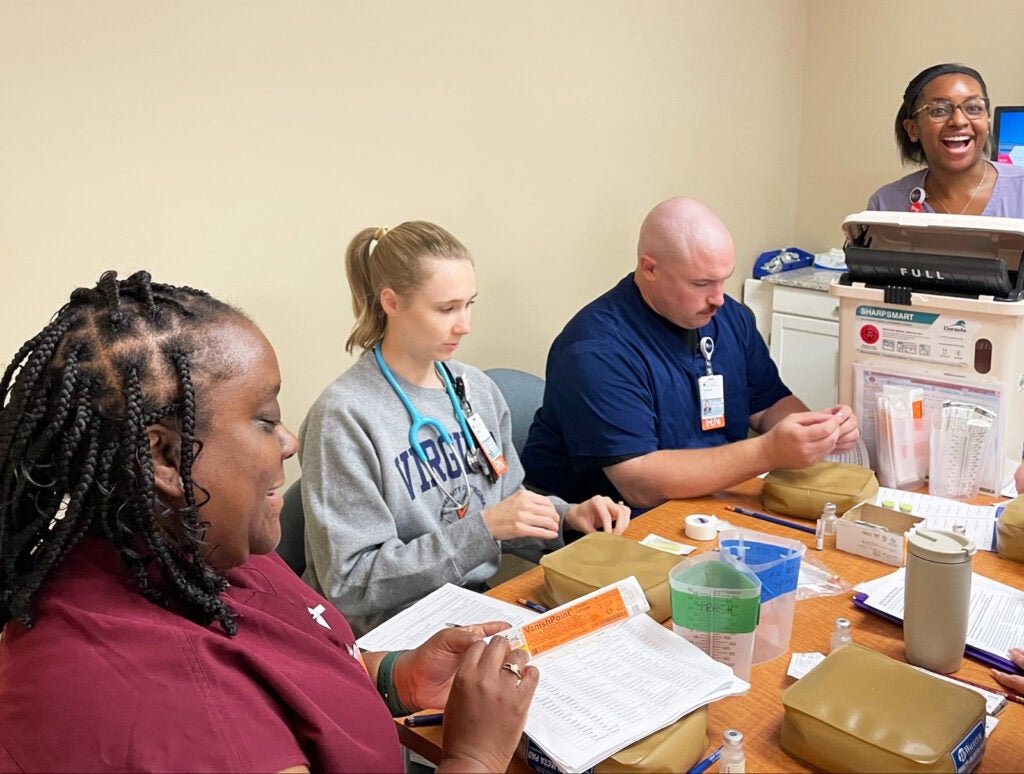
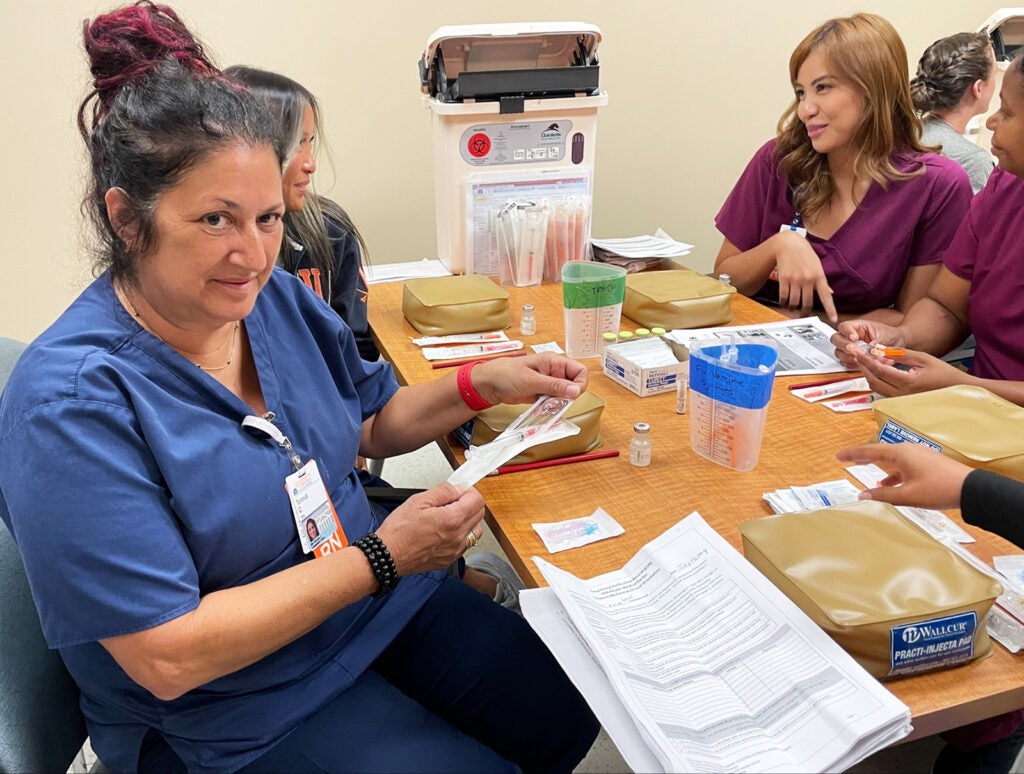
Ronni Rothwell, DNP, MSN, RN, CNE, Nurse Residency Program Manager: Another new component of the program is that it is now two weeks instead of one and we are incorporating simulations. We have a great new simulation center set up at Northridge where we are teaching hands-on basic skills.
Aisha Muhammad, MSN, RN, Nursing Professional Development Specialist: One of the big reasons we moved to this model is that we heard from our preceptors they're overloaded. We’re hoping having new hires’ tier one skills already validated will make for a better experience when they get to the floor.
Q: What are some of the benefits of the new orientation program?
Coffey: There’s a clear benefit to the individuals going through the program, who feel a sense of belonging and more prepared to hit the ground running. This onboarding really builds camaraderie, so participants leave having forged solid relationships with their colleagues.
There’s a benefit to patients because their clinical team members are trained the same way and communicate better because they feel like one team.
There’s a benefit to preceptors, who can welcome their new colleagues with a sense of safety and basic clinical competence established. We are now signing off individuals on upward of 40 distinct competency statements before they enter their patient care area.
I think there's also a benefit to the institution at large because we’ve created more of a community approach. We’ve knocked down perceived walls that prevented teams from sharing in the same goal of welcoming our new team members. We all want an engaged and welcoming work environment — no matter our role or position within our large organization.
Q: Do you foresee making any changes to the program in the future?
Shreckhise: At our simulation center, we are collaborating with the Mayo Clinic to adopt a tiered skills acquisition model (TSAM). We’re starting with tier one skills universal for all patient care. We want all team members to be trained the same way on infection control, vitals and assessment, basic wound care, medication administration, sharps, and safety skills.
Coffey: We're exercising continuous process improvement to optimize the experience of the new hire for Central Clinical Orientation. For example, our Northridge skills days have been restructured to include an expedited experienced nurse track, which accounts for their prior skills to allow for a reduced time requirement. Clinician 1s and internationally-educated nurses have more time for competency validation over a two-day period. This new process has been a real satisfier.
Deanna Pototschnik, MSN, RN, CCRN, Nursing Professional Development Specialist: This is a work in progress, but the main point is that we want lifers — and that starts on day one with orientation. We want UVA Health to be the place where team members feel welcomed and inspired and supported as they progress through their career at UVA Health!
Latest News